It’s the dark cloud on the horizon for the NCAA: Concussions. Two former NCAA athletes are already suing the NCAA over its handling of concussions, and with a U.S. District Judge rejecting the NFL’s $765 million settlement with its players, many speculate that a similar day in court could be had for the NCAA.
But how is a concussion defined? What contributes to adverse health effects from head injuries? Here is all you wanted to know about head injuries and concussions:
Head Injury
What is a head injury?
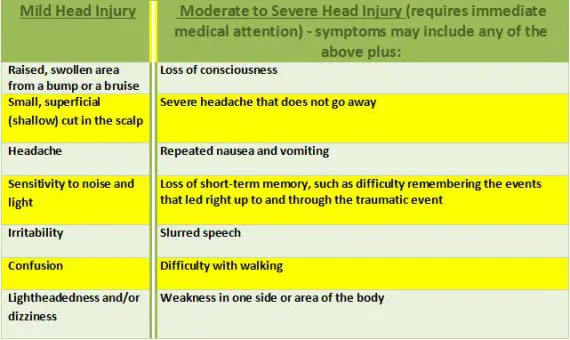
Head injuries are one of the most common causes of disability and death in adults. The injury can be as mild as a bump, bruise (contusion), or cut on the head, or can be moderate to severe in nature due to a concussion, deep cut or open wound, fractured skull bone(s), or from internal bleeding and damage to the brain.
A head injury is a broad term that describes a vast array of injuries that occur to the scalp, skull, brain, and underlying tissue and blood vessels in the head. Head injuries are also commonly referred to as brain injury, traumatic brain injury (TBI), or minimal traumatic brain injury (MTBI) depending on the extent of the head trauma.
Head injuries are rising dramatically, with around 1.47 million injured per year – about 52,000 of those dying. Five million Americans are alive today who have had a head injury and now need help with the activities of daily living, costing the country more than $56 billion per year.
What are the different types of head injury?
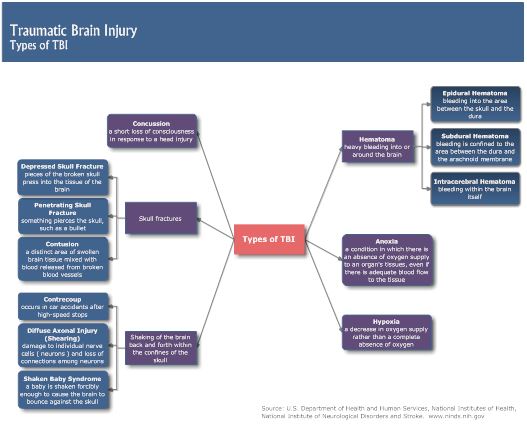
The following are some of the different types of head injuries:
· Concussion:
A concussion is an injury to the head area that may cause instant loss of awareness or alertness for a few minutes up to a few hours after the traumatic event.
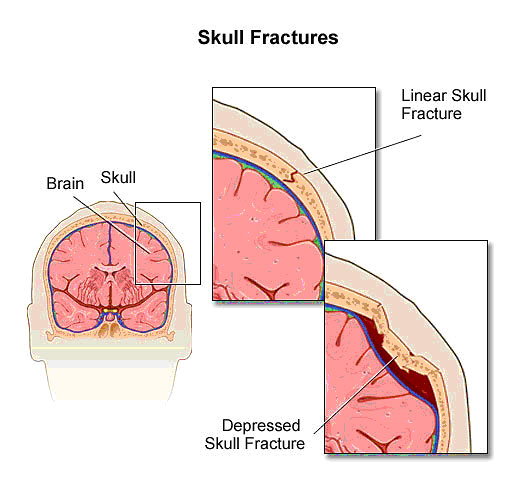
· Skull fracture:
A skull fracture is a break in the skull bone. There are four major types of skull fractures, including the following:
• Linear skull fractures
This is the most common type of skull fracture. In a linear fracture, there is a break in the bone, but it does not move the bone. These patients may be observed in the hospital for a brief amount of time, and can usually resume normal activities in a few days. Usually, no interventions are necessary.
•Depressed skull fractures
This type of fracture may be seen with or without a cut in the scalp. In this fracture, part of the skull is actually sunken in from the trauma. This type of skull fracture may require surgical intervention, depending on the severity, to help correct the deformity.
•Diastatic skull fractures
These are fractures that occur along the suture lines in the skull. The sutures are the areas between the bones in the head that fuse when we are children. In this type of fracture, the normal suture lines are widened. These fractures are more often seen in newborns and older infants.
•Basilar skull fracture
This is the most serious type of skull fracture, and involves a break in the bone at the base of the skull. Patients with this type of fracture frequently have bruises around their eyes and a bruise behind their ear. They may also have clear fluid draining from their nose or ears due to a tear in part of the covering of the brain. These patients usually require close observation in the hospital.
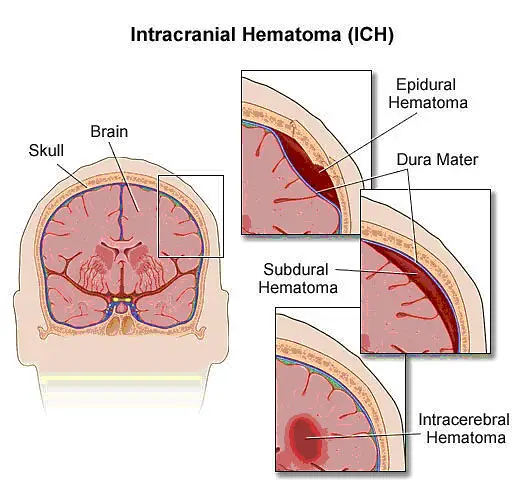
•Intracranial hematoma (ICH)
There are several types of ICH, or blood clots, in or around the brain. The different types are classified by their location in the brain. These can range from mild head injuries to quite serious and potentially life-threatening injuries. The different types of ICH include the following:
•Epidural hematoma
Epidural hematomas occur when a blood clot forms underneath the skull, but on top of the dura, the tough covering that surrounds the brain. They usually come from a tear in an artery that runs just under the skull called the middle meningeal artery. Epidural hematomas are usually associated with a skull fracture.
•Subdural hematoma
Subdural hematomas occur when a blood clot forms underneath the skull and underneath the dura, but outside of the brain. These can form from a tear in the veins that go from the brain to the dura, or from a cut on the brain itself. They are sometimes, but not always, associated with a skull fracture.
•Contusion or intracerebral hematoma
A contusion is a bruise to the brain itself. A contusion causes bleeding and swelling inside of the brain around the area where the head was struck. Contusions may occur with skull fractures or other blood clots such as a subdural or epidural hematoma. When bleeding occurs inside the brain itself (also called “intraparenchymal hemorrhage”), this can sometimes occur spontaneously. When trauma is not the cause, the most common causes are long-standing high blood pressure in older adults, bleeding disorders in either children or adults, or the use of medications that cause blood thinning or certain drugs of abuse.
•Diffuse axonal injury (DAI)
These injuries are common and are usually caused by shaking of the brain back and forth, which can happen in car accidents, from falls or shaken baby syndrome. Diffuse injuries can be mild, such as with a concussion, or may be very severe, as in diffuse axonal injury (DAI). In DAI, the patient is usually in a coma for a prolonged period, with injury to many different parts of the brain.
What causes a head injury?
There are many causes of head injury in children and adults. The most common traumatic injuries are from motor vehicle accidents (automobiles, motorcycles, or struck as a pedestrian), from violence, from falls, or as a result of child abuse. Subdural hematomas and brain hemorrhages (the so-called “intraparenchymal hemorrhages”) can sometimes happen spontaneously.
What causes bruising and internal damage to the brain?
When there is a direct blow to the head, shaking of the child (as seen in many cases of child abuse), or a whiplash-type injury (as seen in motor vehicle accidents), the bruising of the brain and the damage to the internal tissue and blood vessels is due to a mechanism called coup-contrecoup. A bruise directly related to trauma, at the site of impact, is called a coup lesion (pronounced COO). As the brain jolts backwards, it can hit the skull on the opposite side and cause a bruise called a contrecoup lesion. The jarring of the brain against the sides of the skull can cause shearing (tearing) of the internal lining, tissues, and blood vessels that may cause internal bleeding, bruising, or swelling of the brain.
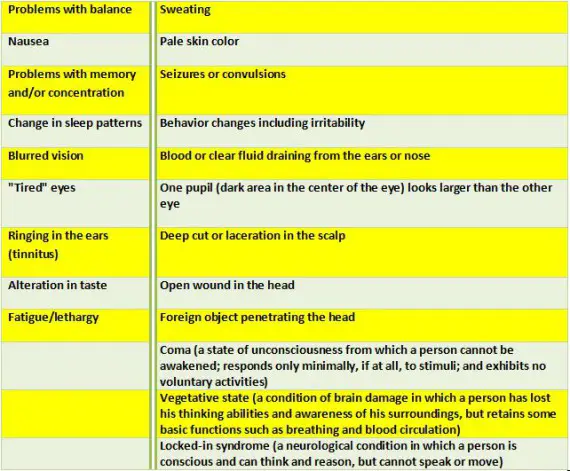 *The symptoms of a head injury may resemble other problems or medical conditions. Always consult your physician for a diagnosis.
*The symptoms of a head injury may resemble other problems or medical conditions. Always consult your physician for a diagnosis.
How are head injuries diagnosed?
The full extent of the problem may not be completely understood immediately after the injury, but may be revealed with a comprehensive medical evaluation and diagnostic testing. The diagnosis of a head injury is made with a physical examination and diagnostic tests. During the examination, the physician obtains a complete medical history of the patient and family and asks how the injury occurred. Trauma to the head can cause neurological problems and may require further medical follow up.
Diagnostic tests may include:
· Blood tests
· X-ray – a diagnostic test that uses invisible electromagnetic energy beams to produce images of internal tissues, bones, and organs onto film.
· Computed tomography scan (Also called a CT or CAT scan.) – a diagnostic imaging procedure that uses a combination of x-rays and computer technology to produce cross-sectional images (often called slices), both horizontally and vertically, of the body. A CT scan shows detailed images of any part of the body, including the bones, muscles, fat, and organs. CT scans are more detailed than general x-rays.
· Electroencephalogram (EEG) – a procedure that records the brain’s continuous, electrical activity by means of electrodes attached to the scalp.
· Magnetic resonance imaging (MRI) – a diagnostic procedure that uses a combination of large magnets, radiofrequencies, and a computer to produce detailed images of organs and structures within the body.
Treatment of a head injury:
Specific treatment of a head injury will be determined by your physician based on:
· Age, overall health, and medical history
· Extent of the head injury
· Type of head injury
· Tolerance for specific medications, procedures, or therapies
· Expectations for the course of the head injury
· Patient’s opinions or preferences
Depending on the severity of the injury, treatment may include:
· Ice
· Rest
· Topical antibiotic ointment and adhesive bandage
· Observation
· Immediate medical attention
· Stitches
· Hospitalization for observation
· Moderate sedation or assistance with breathing that would require being placed on a breathing machine, or mechanical ventilator or respirator
· Surgery
Treatment is individualized, depending on the extent of the condition and the presence of other injuries. If the patient has a severe head injury, he/she may require monitoring for increased intracranial pressure (pressure inside the skull). Head injury may cause the brain to swell. Since the brain is covered by the skull, there is only a small amount of room for it to swell. This causes pressure inside the skull to increase, which can lead to brain damage.
Life-long considerations for a person with a head injury:
The key is to promote a safe environment for children and adults and to prevent head injuries from occurring. The use of seat belts when riding in the car and helmets (when worn properly) for activities such as bicycle riding, in-line skating, and skateboarding may protect the head from sustaining severe injuries.
Persons who suffer a severe brain injury may lose part(s) of muscle, speech, vision, hearing, or taste function, depending on the area of brain damage. Long- or short-term changes in personality or behavior may also occur. These persons require long-term medical and rehabilitative (physical, occupational, or speech therapy) management.
The extent of the person’s recovery depends upon the type of brain injury and other medical problems that may be present. It is important to focus on maximizing the person’s capabilities at home and in the community. Positive reinforcement will encourage the patient to strengthen his/her self-esteem and promote independence.
Concussion and Mild TBI
What is a Concussion?
 A concussion is a type of traumatic brain injury, or TBI, caused by a bump, blow, or jolt to the head that can change the way your brain normally works. Concussions can also occur from a fall or a blow to the body that causes the head and brain to move quickly back and forth.
A concussion is a type of traumatic brain injury, or TBI, caused by a bump, blow, or jolt to the head that can change the way your brain normally works. Concussions can also occur from a fall or a blow to the body that causes the head and brain to move quickly back and forth.
Health care professionals may describe a concussion as a “mild” brain injury because concussions are usually not life-threatening. Even so, their effects can be serious.
What are the Signs and Symptoms of Concussion?
Most people with a concussion recover quickly and fully. Nevertheless, for some people, symptoms can last for days, weeks, or longer. In general, recovery may be slower among older adults, young children, and teens. Those who have had a concussion in the past are also at risk of having another one and may find that it takes longer to recover if they have another concussion.
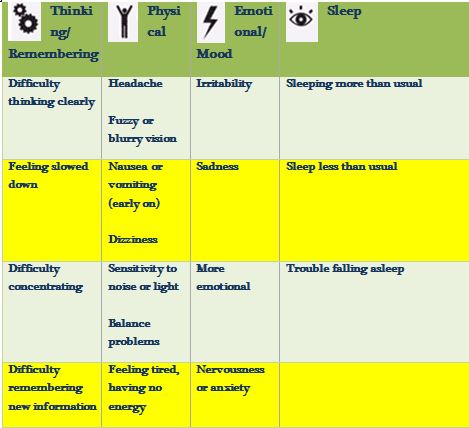
Symptoms of concussion usually fall into four categories:
Some of these symptoms may appear right away, while others may not be noticed for days or months after the injury, or until the person starts resuming their everyday life and more demands are placed upon them. Sometimes, people do not recognize or admit that they are having problems. Others may not understand why they are having problems and what their problems really are, which can make them nervous and upset.
The signs and symptoms of a concussion can be difficult to sort out. Early on, the patient with the concussion, family members, or doctors may miss problems. People may look fine even though they are acting or feeling differently.
When to Seek Immediate Medical Attention:
Danger Signs in Adults
In rare cases, a dangerous blood clot may form on the brain in a person with a concussion and crowd the brain against the skull. Contact your health care professional or emergency department right away if you have any of the following danger signs after a bump, blow, or jolt to the head or body:
· Headache that gets worse and does not go away.
· Weakness, numbness or decreased coordination.
· Repeated vomiting or nausea.
· Slurred speech.
The people checking on you should take you to an emergency department right away if you:
· Look very drowsy or cannot be awakened.
· Have one pupil (the black part in the middle of the eye) larger than the other.
· Have convulsions or seizures.
· Cannot recognize people or places.
· Are getting more and more confused, restless, or agitated.
· Have unusual behavior.
· Lose consciousness (a brief loss of consciousness should be taken seriously and the person should be carefully monitored).
Danger Signs in Children
Take your child to the emergency department right away if they received a bump, blow, or jolt to the head or body, and:
· Have any of the danger signs for adults listed above.
· Will not stop crying and cannot be consoled.
· Will not nurse or eat.
Getting Better
Rest is very important after a concussion because it helps the brain to heal. Ignoring symptoms and trying to “tough it out” often makes symptoms worse. Be patient because healing takes time. Only when symptoms have reduced significantly, in consultation with your doctor, should you slowly and gradually return to your daily activities, such as work or school. If your symptoms come back or you get new symptoms as you become more active, this is a sign that you are pushing yourself too hard. Stop these activities, and take more time to rest and recover. As the days go by, you can expect to feel better gradually.
Tips to help you get better:
· Get plenty of sleep at night, and rest during the day.
· Avoid activities that are physically demanding (e.g., sports, heavy housecleaning, working-out) or require a lot of concentration (e.g., sustained computer use, video games).
· Ask the doctor when the patient can safely drive a car, ride a bike, or operate heavy equipment.
· Do not drink alcohol. Alcohol and other drugs may slow your recovery and put you at risk of further injury.
Many people are available to help you and your family as you recover from a concussion. You do not have to do it alone. Keep talking with your doctor, family members, and loved ones about how you are feeling, both physically and emotionally. If you do not think you are getting better, tell your doctor.
GO DUCKS!
Related Articles:
Chip Kelly Update: Everything's Good Again ...
Chip Kelly Update: Wailing and Gnashing of Teeth
Shock and Awe -- The Oregon Ducks' Football Hangover Effect
Despite Lopsided Score, Georgia State "Never Stopped Believing"
Hope Springs Eternal for Ducks
Incompetent Pac-12 Officials: How Do You Miss ALL of THIS?
NeuroDocDuck (Dr. Driesen) is a doctor who specializes in neurology, and sports medicine. He is an Oregon alumnus, completing his medical education and training in the UK. He has been both a practicing clinician and professor, a well-known and respected diagnostician, an author, and has appeared on national television.
NeuroDocDuck is active in his profession, and stays current on all new trends in his field. He enjoys golf and loves his Ducks!